The short answer to that question: not yet. There is a major problem in developing eye drops for AMD. One article states it as “Ophthalmic drugs have traditionally been administered topically, which in general provides therapeutic levels to the anterior (front) chamber of the eye but not to the Continue reading “UPDATED: Are there eye drops instead of injections to treat wet AMD?”
Category: Highlight
Highlight: What is Myopic Macular Degeneration?
There are quite a few eye diseases that cause degeneration of the macula. The most common forms of macular degeneration are defined by age, at least in part: 1) Age-Related MD (AMD or ARMD) and 2) Juvenile MD (JMD) – several inherited and rare diseases that affect children and young adults including Stargardt’s Disease, Best Disease, and juvenile retinoschisis.
There is another form of macular degeneration called Myopic Macular Degeneration or Myopic Maculopathy.
What is myopia?
If you have trouble seeing things far away like road signs, your eye doctor may have said that means you are nearsighted because you can see things near better than far. Some people call it being shortsighted. The medical/optical term is myopia.
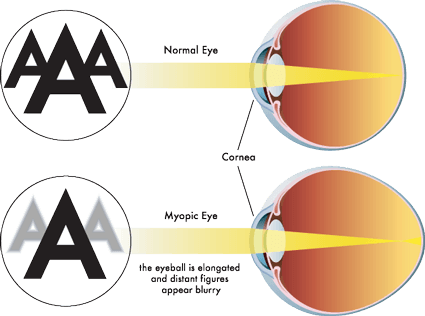
Myopia occurs when the eyeball is too long relative to the focusing power of the cornea and lens of the eye (see diagram above). This causes light rays to focus at a point in front of the retina, rather than directly on its surface. It can also be caused by the cornea and/or lens being too curved for the length of the eyeball. In some cases, myopia is due to a combination of these factors. Click here for more information.
There are different degrees of myopia: mild, moderate and high (also called pathological myopia). The higher the degree, the higher chance of the degeneration of the macula. Click here for some other risks for high myopia including retinal detachment, macular detachment, glaucoma and macular holes.
Myopic Macular Degeneration
People with high myopia/pathological myopia are at risk for damage to the macula from the stretching of it as the eyeball grows throughout life. Here’s a good description of what happens: “As the eyeball grows and stretches, it may also cause an area of atrophy and/or cracks in the layers under the retina. These cracks can serve as conduits for abnormal blood vessels to grow under the retina. These vessels can hemorrhage and scar which is similar to what happens in wet macular degeneration. The onset of the nets of abnormal blood vessels, called Fuch’s spots, often occur in the 4th to 6th decades of life. Approximately 5% of pathological myopia patients develop Fuch’s spots, which lead to damage in the macular region of the eye and a subsequent loss of central vision.” From http://www.lowvision.org/Pathological%20Myopia.htm
Not all people who are myopic get Myopic Macular Degeneration.
Click here for an explanation of how the atrophy can occur as well as how the blood vessels grow into the macula.
The symptoms are similar to AMD & JMD as well. Click here to learn more about them. This article will take you to stories of people who have Myopic MD.
Click here for a first-hand account of the disease from a person with it.
Other links:
American Academy of Ophthalmology Diagnosis and Treatment of CNV in Myopic Macular Degeneration
Treatment Patterns for Myopic Choroidal Neovascularization in the United States, article published July 2017 edition of AAO Journal (AAO is American Academy of Ophthalmologists).
Highlight: Does wet AMD start as dry?
There are differing opinions and interpretations of what those in the field of macular degeneration have learned. The links below certainly don’t represent all views, of course, but are an example of some of what you will find.
The important point is that it is CRITICAL to get your eyes examined as recommended by your doctor and to monitor your vision between exams. Click here to find out how to do that.
From: http://www.webrn-maculardegeneration.com/macular-degeneration-stages.html
“Advanced AMD is either a break-down of light sensitive cells and supporting tissue in the central retinal area (advanced dry form), or the development of abnormal and fragile blood vessels under the retina (wet form).”
From: https://www.macular.org/dry-vs-wet-macular-degeneration
“About ten percent of all cases of Age-related Macular Degeneration become “Wet” AMD (typically a person has dry AMD first and progresses toward wet).”
From: https://nei.nih.gov/health/maculardegen/armd_facts
“There are three stages of AMD defined in part by the size and number of drusen under the retina. It is possible to have AMD in one eye only, or to have one eye with a later stage of AMD than the other.
Early AMD. Early AMD is diagnosed by the presence of medium-sized drusen, which are about the width of an average human hair. People with early AMD typically do not have vision loss.
Intermediate AMD. People with intermediate AMD typically have large drusen, pigment changes in the retina, or both. Again, these changes can only be detected during an eye exam. Intermediate AMD may cause some vision loss, but most people will not experience any symptoms.
Late AMD. In addition to drusen, people with late AMD have vision loss from damage to the macula. There are two types of late AMD:
In geographic atrophy (also called dry AMD), there is a gradual breakdown of the light-sensitive cells in the macula that convey visual information to the brain, and of the supporting tissue beneath the macula. These changes cause vision loss.
In neovascular AMD (also called wet AMD), abnormal blood vessels grow underneath the retina. (“Neovascular” literally means “new vessels.”) These vessels can leak fluid and blood, which may lead to swelling and damage of the macula. The damage may be rapid and severe, unlike the more gradual course of geographic atrophy. It is possible to have both geographic atrophy and neovascular AMD in the same eye, and either condition can appear first.”
From: http://www.avruc.com/macular-degeneration.php
“The macula is the central part of the retina and allows us to read fine print clearly and see colors vividly. It is this area of the retina that deteriorates in ARMD. There are 2 forms of ARMD. Everyone who has macular degeneration starts out with the dry type and 20% progress to the wet type over the course of a lifetime. “
From: http://www.youreyes.org/eyehealth/macular-degeneration
“Can the dry form turn into the wet form?
Yes. All people who had wet form AMD had the dry form first.
The dry form can advance and cause vision loss without turning into the wet form. The dry form also can suddenly turn into the wet form, even during early stage AMD. There is no way to tell if or when the dry form will turn into the wet form.
Can advanced AMD be either the dry form or the wet form?
Yes. Both the wet form and the advanced dry form are considered advanced AMD. Vision loss occurs with either form. In most cases, only advanced AMD can cause vision loss.
People who have advanced AMD in one eye are at especially high risk of developing advanced AMD in the other eye.”
Please see your doctor for regular exams and between exams, check your vision at home.
Highlight: I have drusen, does that mean I have macular degeneration?
Answers
“No, not necessarily. About 50% of the population will show hard drusen and almost 100% the population above 50 will have at least one druse, but many will not develop macular degeneration. An examination by your doctor will help you better understand your risk and what to do about treatment.”
“Not necessarily. Many individuals with some drusen do not go on to develop the visual symptoms of ARMD. From a clinical standpoint, drusen must attain a threshold in numbers, size, and shape for them to become a matter of concern to ophthalmologists.” This article goes on to talk about drusen at the various stages of AMD, the difference between hard and soft drusen and can you prevent, slow down or reverse AMD.
Article answers: what are drusen, types of drusen and questions for your doctor.
Highlight: Is there a connection between drugs taken for osteoporosis and wet AMD?
Click here for the article “A Troubling Link Between osteoporosis Drugs and Macular Degeneration.” There MAY be a link but this article says “Despite the finding, Dr. Etminan, a pharmacological epidemiologist in the Department of Ophthalmology and Visual Science, cautions that it’s too soon for people to stop using the drugs or to avoid taking them, because this is the first study to show a link. Other large-scale studies using other patient databases need to be done before drawing firm conclusions.”
Other Articles
Click here for article “Oral Bisphosphonate Use Poses Risk of Wet AMD”
Click here for article “Examining the Link Between Osteoporosis Drugs and AMD”
Click here for article “Bone Meds Fosamax Boniva Linked to Blinding Macular Degeneration”
Update: Where can I get financial help for the shots I need for my wet AMD?
One of the members of our Facebook group shared with us information about a Patience Assistance Network (PAN) Foundation (US) which has helped her to pay for shots when her insurance would not pay. PAN’s purpose is to “help under-insured people with life-threatening, chronic and rare diseases get the medications and treatment they need by paying for their out-of-pocket costs and advocating for improved access and affordability.” To qualify, you must be within their income guidelines and the medication must be on their list. This program applies to more than just medications related to vision.
Click here to find out more about the PAN Foundation. Their available funding fluctuations so you may have to check with them regularly.
Click here for a list of other Patient Support organizations including from the companies who make Lucentis and Avastin.
Click here for the company who makes Eylea.
Click here for a company in the US called GoodDays.
Click here for a list for assistance with the medications as well as with other expenses.
In the US, you may also qualify for Social Security Disability which would give you a monthly income and Medicare benefits. Click here for that information.
Please contact me directly (light2sight5153@gmail.com) or leave a comment on this page if:
- you live in the US and have experience with any of these organizations
- you live outside the US and know of any similar organizations in your country
updated 12/13/2016
Updated: Is there a relationship between cataracts and macular degeneration?
Disclaimer: I’m NOT a medical person & this isn’t advice. I do research on topics & summarize what I find to try to make it more understandable. –Linda…
What is a cataract?
“A cataract is a cloudy or opaque area in the normally clear lens of the eye. Depending upon its size and location, it can interfere with normal vision. Most cataracts develop in people over age 55, but they occasionally occur in infants and young children. Usually cataracts develop in both eyes, but one may be worse than the other.” From Glossary of Eye and Vision Conditions
Here’s a good video from the National Eye Institute “Cataracts”
Here’s a very comprehensive website section with not only statistics from the UK but also sections on what they are, what medications are used with them, and where you can get more information.
Cataract removal in someone with AMD
Question is how much of one’s poor vision is from the cataract & how much from the AMD? Depends on the severity of the cataract & stage of the AMD.
Possible Benefits
From Cataracts & Age-Related Macular Degeneration
- if it’s mild AMD, cataract removal may improve acuity even of central vision.
- if more advanced AMD, removal may help with color discrimination, contrast, clarity or peripheral vision.
- if it’s wet AMD which hasn’t been stabilized, see ‘Risks’ below.
- if it’s a thick cataract that prevents the doctor from seeing the macula clearly especially if there’s a high risk for wet AMD, removal may aid the doctor in accurate diagnosis of condition of the macula.
Risks of cataract removal in someone with AMD
Basically the same as those without AMD except when the AMD is not stabilized – more below. In general, it’s considered to be a low-risk procedure.
Considerations:
- the natural lens (that’s what turns yellow and is called a cataract) filters blue light but you can get an IOL (Intraocular Lens) that will help to filter some of it out (no evidence this reduces vision).
- risk of Posterior Vitreous Detachment (PVD) which can result in floaters or retinal holes or retinal detachments (holes or detachments can occur in the macula).
- inflammation related to AMD. Solution: pre-op NSAIDS (anti-inflammatories).
- From Cataract Surgery in the Patient with AMD
“Additionally, growing evidence supports a pathogenic role for inflammation in AMD, and the normal inflammatory response that accompanies cataract surgery, even when uncomplicated, may be deleterious to at-risk eyes. However, epidemiologic studies to date have failed to prove definitively that cataract surgery is associated with AMD progression. “ - From Cataract Surgery in the Patient with AMD “In summary, in the patient with a visually significant cataract, AMD should not be considered a contraindication to cataract surgery, and surgery need not be delayed for fear of causing advanced AMD. Factors such as IOL selection and peri-operative management may optimize visual outcome and reduce the risk of AMD progression.
- From Cataract Surgery in the Patient with AMD
Other references:
Cataracts and Macular Degeneration from WebRN-MacularDegeneration.com
The Impact of Cataract Surgery on Pre-existing Retinal Disease
updated 1/27/2017
About our Project 7/31/2016
We’ve had some people (and you know who you are ::smile::) ask about what goes on ‘behind the scenes’ with our project so I’ve written a page about just that.
Highlight: Once my wet AMD is stabilized, does my eye continue to worsen?
There’s been some confusion in what eye doctors have told patients about the disease process in AMD and there are 2 questions that have come up in the Facebook group: 1) does wet AMD start as dry? 2) once the bleeding is stopped in the wet form, does the deterioration of the macula continue, ie, does the dry process continue?
About question 1, through my research I’ve found that a lot of articles don’t specify this, they just say there is the wet kind and the dry kind. However, most descriptions from reliable sources say YES, wet AMD starts as dry but sometimes the dramatic symptoms from the bleeding gets a person to the eye doctor & they never got the diagnosis of dry where the early stage has few symptoms.
About number 2, here’s the clearest answer to that question I can find:
Click here for the full article. There is at least one error in the transcript. In the second paragraph of Dr. Gorin’s response that starts with “We understand a great deal more in recent years because of the genetics studies that have been done.”, there is the word ‘bruising’ which should be ‘drusen’.
In this article, here is a quote is from the transcript of a telephone discussion with Michael B. Gorin, MD, PhD, an ophthalmologist from UCLA who is devoted to research and clinical care of hereditary retinal disorders, especially age-related macular degeneration, retinal dystrophies and other medical retinal conditions.
Dr. Gorin:
“But for a group of patients, it can diverge into two different paths of progression. One is where the cells that care for the retina begin to die and you start getting areas of atrophy—that is, cell loss—and on those areas of cell loss, you lose areas of vision. And that’s called atrophic, or advanced dry macular degeneration. That’s usually slower, but it can be very problematic for people, because it can create little holes in their vision and ultimately, if those holes get larger and coalesce, one can lose central vision from that. The second pathway—and by the way, they are not mutually exclusive, some people can have both of these things going on—is because of the damage to the cells underneath the retina, it triggers the formation of a blood vessel, either a blood vessel underneath the retina or sometimes even in the retina. That blood vessel is an abnormal growth; it’s not a tumor or a cancer, but it’s a blood vessel that’s stimulated to grow, and it unfortunately leaks and can bleed, and because of that leakage and bleeding, you get the term ‘wet’, because the fluid is leaking into the retina. Over time, that accumulation of blood and fluid disrupts not only the architecture of the cells, but can lead to fairly rapid vision loss. So, wet macular degeneration treatments at this stage are really focused on trying to prevent the ongoing growth and leakage of these abnormal blood vessels. The treatments do not stop the underlining degenerative process or the causes of macular degeneration in the first place. A person who is having successful treatment of the wet form of macular degeneration is really not having their macular degeneration stopped. The treatment is blocking and limiting the amount of damage that occurs.”
Highlight: Why are you taking that?
June 24, 2016
I have published information about the AREDS/AREDS2 supplements in the past. In the Facebook group, we’ve discussed the studies and the pros and cons of taking the supplements. Here’s the text of an article that I hope will clarify some of the concerns that have been expressed by eye professional. The link to the article is at the end of this post.
A long-time patient presented for an exam the other day. This is a patient that I look forward to seeing, as we have some common interests that we chat about during his exam. He remarked that he really enjoyed coming for his exam, because he felt secure in the advice I give him. However, he also stated he has recently experienced an unsettled feeling in having to find a new primary care provider due to insurance changes.
Here’s a bit of history on this patient: He is in his mid-50s, myopic, but otherwise enjoys normal ocular health. He has a family history of age-related macular degeneration, with both his mother and maternal aunt having undergone anti-VEGF injections for wet AMD. Several years ago I measured his macular pigment optical density and found it to be very low. I prescribed a triple carotenoid supplement (lutein, zeaxanthin and mesozeaxanthin), his pigment level is now well within normal range, and he reports taking this supplement without fail. In reviewing his medications, I noticed an addition, an Age-Related Eye Disease Study 2 formula. Knowing I had not prescribed this, I asked him why he was taking it.
“Well, I was at the drugstore and saw the box. It said that it was the No. 1 doctor-recommended brand, and the only clinically proven formula, so I thought I would take this along with what you prescribed. It is only a vitamin right?”
Only a vitamin… So this patient who has stated he trusts what I recommend for his eyes has fallen prey to misleading advertising on a product label at his local pharmacy.
I asked him a few questions.
GM: Did the label state that there is no clinically proven benefit to taking the AREDS2 formula for patients without AMD or even those with mild disease, only a moderate benefit for those with intermediate to severe disease?
Patient: Well, no, it did not say that.
GM: Did the label tell you that taking large doses of zinc have been linked to the development of Alzheimer’s disease and prostate cancer?
Patient: No, the label did not say that either.
GM: Did the label state that other studies have found that vitamins C and E have no effect on the development of AMD?
Patient: No.
GM: Did the label state that high doses of vitamin E have been associated with increased risk of heart failure?
Patient: No.
GM: Did the label state that if you have the wrong genetics, the high dosage of zinc might accelerate progression of AMD?
Patient: No.
GM: Do you think I would prescribe this for you?
Patient: No, definitely not. I am throwing away the bottle when I get home!
Interestingly, 2 days after this encounter I read an announcement regarding the release of an AREDS2 formula plus a multivitamin. It was stated that the reason for the combination formula was due to the fact that 90% of participants in the AREDS2 trial that took an AREDS supplement also took a multivitamin (which in itself may have skewed the results of the trial). The piece also stated that consumer feedback and data showed that more than 50% of people older than 50 use a multivitamin.
Unfortunately, supplements do not face the same FDA scrutiny as drugs do. Consider what is seen in TV ads for drugs. The announcer lists a litany of possible side effects that the drug being advertised may have, all the while showing images of the supposed patient taking the drug playing with their grandkids or walking along a beach. Now imagine if a commercial for an AREDS formula vitamin had to do the same. Patients would likely think twice while in the drug store vitamin aisle about self-prescribing. And perhaps maybe they would ask for advice from their eye care provider.
References:
The Age-Related Eye Disease Study 2 Research Group. JAMA.2013;309(19):2005-2015. doi:10.1001/jama.2013.4997.
Awh CC, et al. Ophthalmology. 2015;122(1):162-169; doi: 10.1016/j.ophtha.2014.07.049.
Christen WG, et al. Ophthalmology. 2012;119(8):1642-1649; doi: 10.1016/j.ophtha.2012.01.053.
Leitzmann MF, et al. J Natl Cancer Inst. 2003; 95:1004-1007.\
The article above is from: http://www.healio.com/optometry/nutrition/news/blogs/%7Bcc9498b0-051f-44c9-948d-dac572140054%7D/gary-l-morgan-od/blog-why-are-you-taking-that

