There are quite a few eye diseases that cause degeneration of the macula. The most common forms of macular degeneration are defined by age, at least in part: 1) Age-Related MD (AMD or ARMD) and 2) Juvenile MD (JMD) – several inherited and rare diseases that affect children and young adults including Stargardt’s Disease, Best Disease, and juvenile retinoschisis.
There is another form of macular degeneration called Myopic Macular Degeneration or Myopic Maculopathy.
What is myopia?
If you have trouble seeing things far away like road signs, your eye doctor may have said that means you are nearsighted because you can see things near better than far. Some people call it being shortsighted. The medical/optical term is myopia.
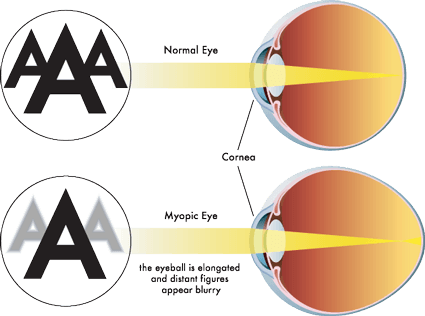
Myopia occurs when the eyeball is too long relative to the focusing power of the cornea and lens of the eye (see diagram above). This causes light rays to focus at a point in front of the retina, rather than directly on its surface. It can also be caused by the cornea and/or lens being too curved for the length of the eyeball. In some cases, myopia is due to a combination of these factors. Click here for more information.
There are different degrees of myopia: mild, moderate and high (also called pathological myopia). The higher the degree, the higher chance of the degeneration of the macula. Click here for some other risks for high myopia including retinal detachment, macular detachment, glaucoma and macular holes.
Myopic Macular Degeneration
People with high myopia/pathological myopia are at risk for damage to the macula from the stretching of it as the eyeball grows throughout life. Here’s a good description of what happens: “As the eyeball grows and stretches, it may also cause an area of atrophy and/or cracks in the layers under the retina. These cracks can serve as conduits for abnormal blood vessels to grow under the retina. These vessels can hemorrhage and scar which is similar to what happens in wet macular degeneration. The onset of the nets of abnormal blood vessels, called Fuch’s spots, often occur in the 4th to 6th decades of life. Approximately 5% of pathological myopia patients develop Fuch’s spots, which lead to damage in the macular region of the eye and a subsequent loss of central vision.” From http://www.lowvision.org/Pathological%20Myopia.htm
Not all people who are myopic get Myopic Macular Degeneration.
Click here for an explanation of how the atrophy can occur as well as how the blood vessels grow into the macula.
The symptoms are similar to AMD & JMD as well. Click here to learn more about them. This article will take you to stories of people who have Myopic MD.
Click here for a first-hand account of the disease from a person with it.
Other links:
American Academy of Ophthalmology Diagnosis and Treatment of CNV in Myopic Macular Degeneration
Treatment Patterns for Myopic Choroidal Neovascularization in the United States, article published July 2017 edition of AAO Journal (AAO is American Academy of Ophthalmologists).
