We have a GREAT Facebook group (as I’m typing, there are 1,898 members, but that will change shortly since I add at least a few new members every day). They share information and ask me questions and also ask questions of other members. That’s one of the reasons that I started the group: to encourage discussion.
A recent discussion of what happens after anti-VEGF injections brought up the confusing use of the word “dry” when talking about wet AMD. Doctors will often tell patients, “Your eye is dry,” or, “Your AMD has dried up.” One of the members said that’s what she was told. Another member asked, “Can wet AMD turn to dry AMD?” Because of the confusing use of the word “dry”, other members said, “Yes!” It turns out that they were mostly referring to the correct use of the word, but I thought it a good time to clarify this.
When the doctor tells you that your wet AMD is now “dry”

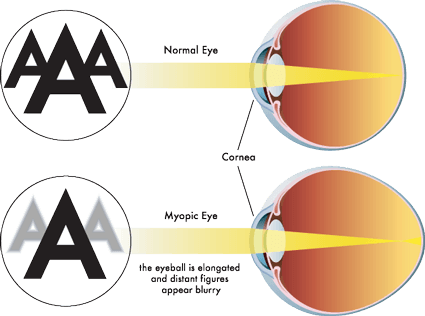
In the diagram, going from left to right is the disease PROCESS from no AMD to dry then to wet AMD. Not everyone gets to the last & wet stage (10-15% of those who have AMD), but if they do, the disease process continues. If the injection was successful, the fluid that was leaking has “dried up.” Do NOT let down your guard thinking you have dry AMD and stop checking your vision or going to the eye specialist. Unfortunately, there is no way to reverse the disease process yet.
Another way to view the process

This diagram is from the most comprehensive page on wet AMD I have found. Some of it is highly technical, but it should give you a sense of what happens when the disease process of AMD progresses to wet. There are no arrows pointing up at the bottom of the diagram. The fluid from wet AMD can ‘dry up’ – that’s the objective – but the disease process does not go back to an earlier stage. Some people will say that if the macula is “dry”/”dried up”, the disease goes “dormant.” Regardless of the terminology, the disease process cannot be reversed yet. The injections treat the symptoms that affect visual acuity.
Another name for wet AMD is CNV which is Choroidal NeoVascularization (CNV is also used in other forms of macular degeneration). The choroid is where the blood vessels are below Bruch’s Membrane and the RPEs and photoreceptors (see the illustration at the top of the page). Neo means “new” and vascularization is abnormal or excessive formation of blood vessels.
Do you have questions about wet AMD?
Of course, we’d love if you’d join the Facebook group, but we know that some of you have chosen not to for various reasons – and that’s okay. If you have questions, please put them in the ‘leave a reply’ section, and I’ll answer them as soon as I can.